Why the Word ‘Benign’ Can Be So Damaging for People with Acoustic Neuromas (and Other Brain Tumours)
When you first hear the word benign after a brain scan, it can sound like a huge relief.
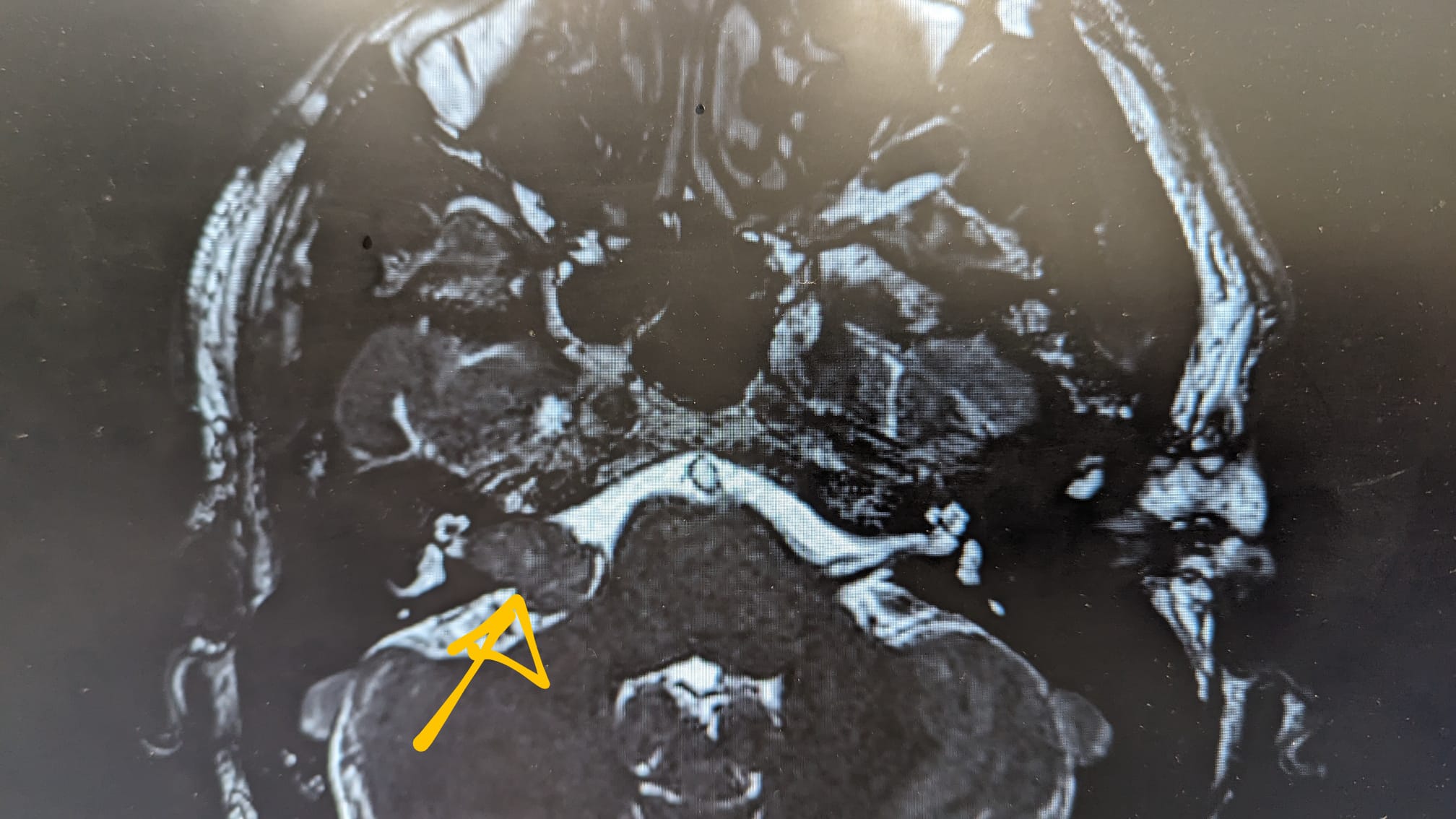
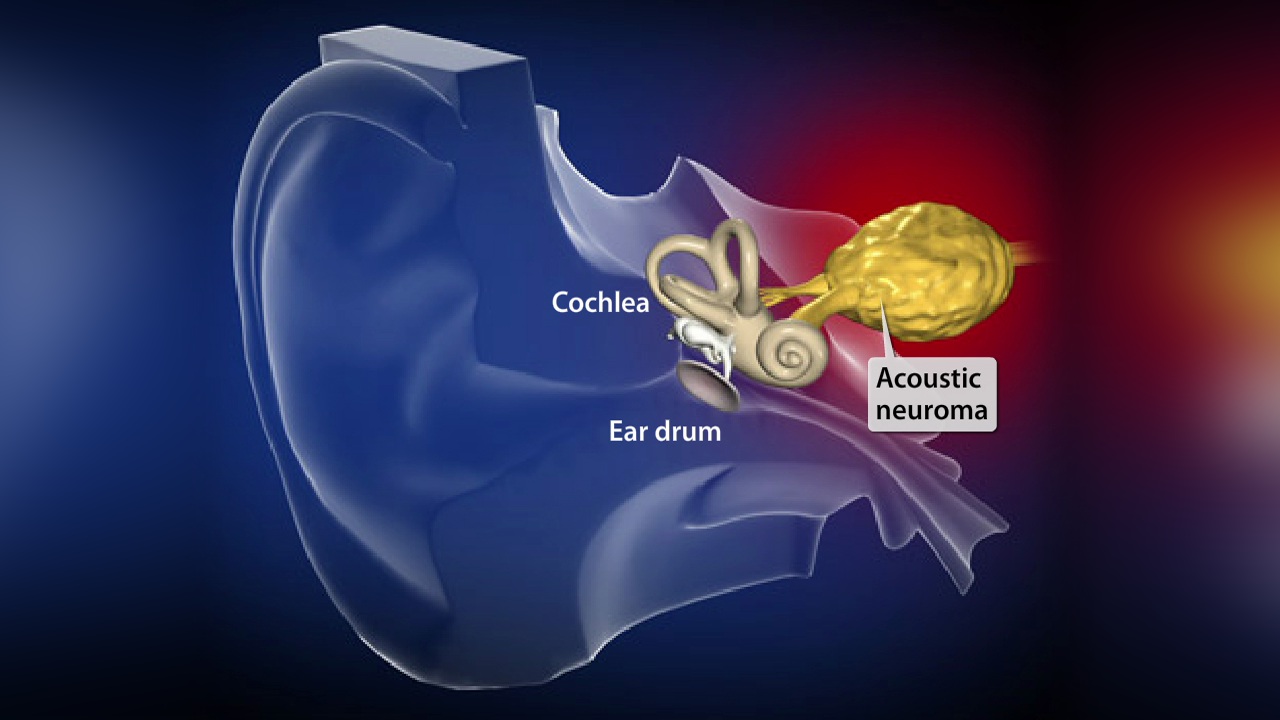
It means your tumour isn’t cancerous. You don’t need chemotherapy. You might not even need surgery. But if you’ve been diagnosed with an acoustic neuroma (also known as a vestibular schwannoma), or another so-called “benign” brain tumour, you’ll quickly discover how deceptive that word can be.
Table Of Content
Because benign doesn’t mean harmless.
For many in the acoustic neuroma community, the effects of the tumour are anything but minor. These tumours may grow slowly—or not at all—but they often cause permanent, life-altering symptoms. From hearing loss and unrelenting tinnitus to balance issues, facial nerve complications, fatigue, and serious mental health challenges, the journey is rarely simple. And even if your tumour is deemed stable or requires only monitoring, you’re often left managing the fallout on your own.
The Problem with the Word “Benign”
In medical terms, “benign” refers to tumours that are not cancerous and do not spread to other parts of the body. But in day-to-day life, the word carries a different weight. It suggests something harmless or inconsequential—something that doesn’t need to be worried about. And that perception is incredibly damaging.
When healthcare professionals, employers, or even family and friends hear benign, the default assumption is that the person is fine. That the diagnosis isn’t serious. That recovery is quick. That life returns to normal.
But the reality is far more complex. Recovery—if treatment is even offered—is often long and incomplete. And for many people, life never returns to how it was before diagnosis. The word benign oversimplifies that reality and risks leaving people overlooked and unsupported.
The Real-World Impact
Living with an acoustic neuroma often means dealing with symptoms that are invisible, persistent, and incredibly disruptive. These can include:
- Permanent hearing loss, often in one ear, making conversation—especially in noisy settings—challenging and isolating.
- Chronic tinnitus, a constant ringing or buzzing that can be distressing, distracting, and emotionally draining.
- Balance problems, which may require physiotherapy or long-term lifestyle changes to manage.
- Cognitive fatigue, which impacts focus, work, memory, and the ability to engage in everyday activities.
- Facial weakness or numbness, sometimes following surgery or radiation treatment.
- Emotional and mental health strain, including anxiety, depression, or post-traumatic stress, especially around follow-up scans and medical appointments.
Even though these effects are well-documented, they are often dismissed because they don’t fit the popular narrative of what a brain tumour “should” look like—especially one labelled benign.
Treatment Isn’t Always a Solution
Whether someone is under active monitoring, has undergone surgery, or received radiation, there’s a common misconception that once the treatment is complete, life will return to normal.
But many people are left with lasting side effects—physical, neurological, and emotional. These can include new mobility issues, speech difficulties, vision or hearing loss, and increased sensitivity to sound and light. Recovery can mean relearning basic tasks, adjusting to new limitations, and accepting that some symptoms may be permanent.
And for those in a “wait and watch” phase, there’s a different kind of mental strain. Living with the knowledge that there’s a tumour in your head, knowing it might grow or change, and attending routine scans can be a constant source of stress.
Mental Health Is Too Often Overlooked
One of the most under-recognised aspects of living with a benign brain tumour is the emotional aftermath. The trauma of diagnosis, treatment decisions, lifestyle changes, and long-term symptoms can have a profound impact on mental health.
It’s not uncommon for people to develop anxiety, depression, or even PTSD after surgery or radiation. There’s also the isolation that comes from having an “invisible” condition. Many feel pressure to downplay their symptoms or avoid talking about their difficulties because they don’t feel they have the right to complain.
Others experience survivor’s guilt, especially when they know others dealing with more aggressive brain tumours. There’s a sense of being caught between two worlds—grateful for a non-malignant diagnosis, yet still carrying the burden of a condition that has deeply changed their life.
The Social Impact: Relationships and Understanding
Relationships can shift dramatically after diagnosis. Some friends and family may not understand the seriousness of a benign brain tumour or struggle to know how to offer support. There can be a sharp drop in help and understanding after the initial diagnosis phase, leaving people feeling forgotten.
In some cases, relationships are strained because of the changes in personality, mood, or energy levels. And when social circles shrink, it can compound feelings of isolation, especially when communication and socialising become more difficult due to hearing loss or fatigue.
Support Is Out There
Despite the challenges, support is available—and it can make a huge difference.
- BANA UK (British Acoustic Neuroma Association) provides a lifeline for many people affected by acoustic neuromas. With resources, patient stories, and community events, it’s a hub of shared experience and understanding.
- The British Acoustic Neuroma Support Group on Facebook is a vibrant online space where thousands of people share tips, ask questions, and offer emotional support to one another.
A Call for Change
It’s time to re-evaluate how we talk about brain tumours like acoustic neuromas. Medical language has consequences—and in this case, calling something “benign” can do more harm than good. It creates a narrative that undermines the reality people live with every day.
We need better understanding, more empathetic healthcare responses, long-term emotional support, and improved access to rehabilitation. We need more research funding and public awareness for benign brain tumours. And we need to make sure no one is made to feel like their experience doesn’t count—just because their diagnosis wasn’t cancer.
Let’s change the language.
Let’s change the outcomes.
Let’s make sure benign is never used to dismiss or diminish someone’s reality.
Because even if it’s benign, it’s still a brain tumour. And that’s never simple.