Using Power BI for Health Analytics in General Practice: Unlocking the Power of Data for Better Patient Outcomes
In today’s fast-paced healthcare environment, General Practices (GPs) must continuously monitor and improve their performance to meet the needs of their patients. This requires robust, data-driven insights into clinical and operational activities. One of the most effective ways to gain these insights is through business intelligence (BI) tools like Microsoft Power BI, which enable healthcare teams to transform raw data into meaningful information. Power BI is increasingly being used in general practice to monitor various health indicators and improve decision-making.
Table Of Content
- The Power of Data in General Practice
- What Power BI Can Do for General Practice
- Appointment Data
- Patient Demographics
- Chronic Disease Management
- Workforce Management
- Financial Performance
- Prescribing Patterns
- Quality of Care Metrics (QOF and CQC Compliance)
- Proactive Care and Patient Engagement
- Benefits of BI Tools in General Practice
- Conclusion
In this article, we will explore the potential of Power BI for health analytics in General Practice, its application for monitoring key performance indicators (KPIs), and how BI tools can benefit practice managers and clinicians.
The Power of Data in General Practice
General practices are sitting on a wealth of patient and operational data. From appointment bookings and clinical outcomes to staff workload and resource management, this data can offer valuable insights when processed effectively. However, many practices struggle to make sense of the data or lack the right tools to interpret it in a way that drives actionable results.
This is where BI tools like Power BI come into play. Power BI provides a user-friendly platform that enables practice managers and healthcare teams to visualise data trends, identify performance gaps, and make more informed decisions.
What Power BI Can Do for General Practice
To truly unlock the power of Power BI in general practice, it’s essential to delve deeper into the individual key performance indicators (KPIs) and metrics that a typical practice would monitor.
These indicators allow practice managers and clinicians to track and assess performance across clinical, operational, and financial areas. In this expanded section, we will explore the core elements of a practice management dashboard.
Appointment Data
- Total Number of Appointments: The total count of all scheduled appointments within a set time period.
- DNA (Did Not Attend) Rate: The percentage of patients who fail to attend their scheduled appointments without prior cancellation.
- Cancellation Rate: The proportion of appointments canceled by patients or the practice.
- Appointment Type Breakdown: A classification of appointments by type (e.g., GP, nurse, telephone consultations, face-to-face, e-consults).
- Appointment Slot Utilisation: The percentage of available appointment slots that are filled, helping to measure efficiency in scheduling.
- Average Wait Time for Appointments: The average waiting time between a patient’s request for an appointment and the time they are seen.
- Urgent vs. Routine Appointments: The ratio of urgent appointments to routine ones, which can help practices manage demand for immediate care.
Why It Matters: High DNA and cancellation rates can indicate inefficiencies, while a low utilisation rate could suggest an underused resource. Tracking these metrics allows practices to adjust schedules, optimise appointment types, and implement reminder systems to reduce DNA rates.
Patient Demographics
- Age Distribution: The proportion of patients across different age groups, such as 0-16, 17-64, and 65+.
- Gender Distribution: The ratio of male to female patients registered at the practice.
- Ethnicity Breakdown: The distribution of patients by ethnic groups, which is essential for ensuring that services are accessible to all demographics.
- Socioeconomic Status (Deprivation Index): Data on the socio-economic backgrounds of patients, often measured using indices like the IMD (Index of Multiple Deprivation).
Why It Matters: Understanding the demographics of the patient population helps the practice tailor services to meet their needs. For example, an elderly population might indicate a need for more chronic disease management or home visits, while a high proportion of younger patients may require a focus on pediatric care.
Chronic Disease Management
- Disease Prevalence Rates: The percentage of patients diagnosed with chronic conditions such as diabetes, hypertension, COPD, asthma, and cardiovascular disease.
- QOF (Quality and Outcomes Framework) Achievement Rates: The practice’s performance on managing chronic diseases according to QOF targets.
- Patient Review Rates: The percentage of patients with chronic conditions who have had their annual reviews or follow-ups within the recommended time frame.
- Medication Adherence: The percentage of patients adhering to their prescribed treatment for chronic diseases.
- Clinical Outcome Measures: Metrics such as blood pressure control in hypertension or HbA1c levels in diabetic patients.
Why It Matters: Effective chronic disease management ensures better health outcomes and reduces hospital admissions. Monitoring these metrics helps practices identify gaps in care and intervene early.
Workforce Management
- Staff Utilisation Rates: The percentage of time clinical and non-clinical staff spend on patient-facing vs. administrative tasks.
- Staff Absenteeism: The rate of staff sickness and absenteeism over time, which can help flag issues related to workforce well-being.
- Patient-to-Clinician Ratio: The number of registered patients per GP, nurse, or clinician, indicating whether staffing levels are appropriate to meet demand.
- Average Consultation Length: The average time spent in consultations, which can indicate pressures on clinicians or the need for additional resources.
- Training and Development Hours: The number of hours clinicians and staff spend on professional development and training.
Why It Matters: Managing workforce metrics helps practices ensure staff are deployed efficiently, reducing burnout while maintaining high-quality care. It also aids in planning for future staffing needs based on patient demand.
Financial Performance
- Total Income by Source: Breakdown of income from different sources such as NHS contracts, enhanced services, private services, and other funding streams.
- Cost per Patient: The total cost of care delivery per patient registered with the practice.
- Revenue per Clinician: The income generated by each clinician, helping practices assess the financial sustainability of their service delivery.
- Expenditure Breakdown: Categorisation of operational expenses such as staff salaries, utilities, medical supplies, and facility maintenance.
- Profit Margins: The percentage of income that translates into profit, indicating the overall financial health of the practice.
Why It Matters: Monitoring financial metrics is essential for the long-term sustainability of the practice. Practices can optimise resource allocation, reduce unnecessary expenses, and forecast future financial needs.
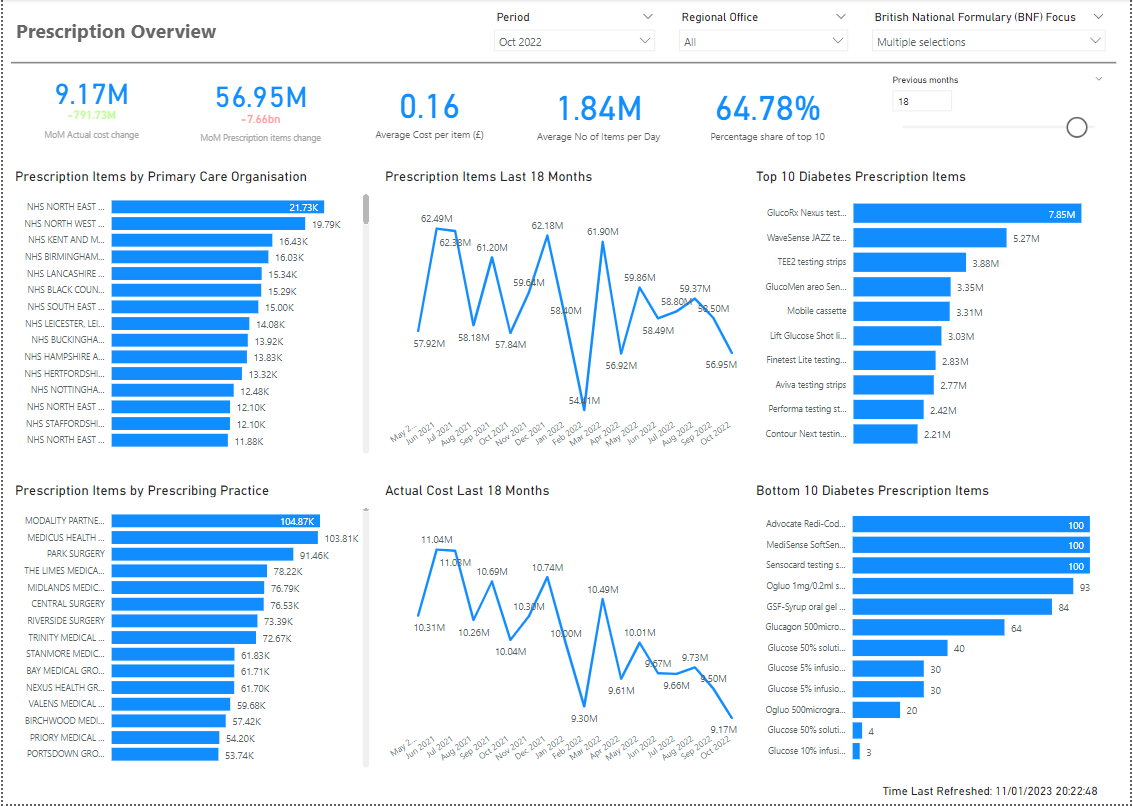
Prescribing Patterns
- Number of Prescriptions Issued: The total number of prescriptions issued in a given time frame, broken down by medication type.
- High-Risk Medication Monitoring: The percentage of patients on high-risk medications (e.g., opioids, anticoagulants) who are regularly reviewed.
- Cost of Prescriptions: The total cost of medications prescribed, which can be compared against budgeted amounts or national benchmarks.
- Medication Compliance: The percentage of patients who follow their prescribed medication regimen.
- Antibiotic Prescribing Rates: The frequency of antibiotic prescriptions, an important metric for monitoring and controlling antimicrobial resistance.
Why It Matters: Controlling prescribing patterns not only helps ensure appropriate medication use but also aligns with national guidelines for cost-effectiveness and safety, such as the NHS’s focus on reducing antibiotic over-prescription.
Quality of Care Metrics (QOF and CQC Compliance)
- QOF Achievement: Percentage of clinical targets achieved under the Quality and Outcomes Framework, which evaluates performance across areas like smoking cessation, flu vaccination, and disease management.
- Patient Safety Indicators: Metrics related to patient safety incidents, significant events, and safeguarding concerns.
- Care Quality Commission (CQC) Compliance: Monitoring adherence to the CQC’s fundamental standards of care, such as ensuring proper infection control, safe medication practices, and safeguarding vulnerable patients.
- Patient Feedback Scores: Ratings and comments from patient satisfaction surveys or the NHS Friends and Family Test (FFT).
Why It Matters: Tracking these indicators ensures that practices meet national standards for quality and safety. Maintaining high QOF scores, for example, can also have financial implications, as practices are rewarded for providing high-quality care.
Proactive Care and Patient Engagement
- Health Screening Rates: Percentage of eligible patients who have received screenings for conditions such as cancer (breast, bowel, and cervical screenings) and cardiovascular risk.
- Vaccination Uptake: The rate of vaccination for routine and seasonal vaccines (e.g., flu, MMR, COVID-19).
- Patient Recall and Follow-Up Rates: The percentage of patients who have been recalled for follow-ups, particularly for chronic disease management, annual reviews, or health checks.
- Patient Portal Utilisation: The percentage of patients actively using digital services such as online booking, repeat prescription requests, and access to medical records.
Why It Matters: Proactive patient engagement is key to preventative care. By monitoring these metrics, practices can ensure that patients are receiving the care they need to stay healthy, preventing more serious conditions from developing.
Benefits of BI Tools in General Practice
Improved Decision-Making
Power BI transforms raw data into clear visualisations, allowing practice managers and clinicians to see patterns and trends in real-time. This facilitates more informed decision-making, particularly when it comes to managing patient care, staff allocation, and financial planning.Enhanced Patient Outcomes
BI tools help track clinical KPIs such as chronic disease management, patient follow-ups, and medication adherence. By staying on top of these metrics, practices can identify patients who require additional care or interventions, leading to better patient outcomes.Operational Efficiency
Practices can optimise their workflows by analysing appointment utilisation and staffing levels. Power BI can highlight bottlenecks or inefficiencies in the system, enabling practices to adjust resources and scheduling for maximum efficiency.Financial Visibility
BI dashboards provide a clear view of financial performance, helping practices to track revenue streams, monitor expenditure, and forecast future income. This ensures that the practice remains financially sustainable while delivering high-quality care.Compliance and Accountability
Using BI tools, practices can monitor their adherence to national and local standards, such as QOF or CQC (Care Quality Commission) requirements. The ability to track these metrics in real-time ensures that practices remain compliant and accountable to regulators and patients alike.Customisable Dashboards
One of the strengths of Power BI is its flexibility. Practices can create customisable dashboards tailored to their specific needs, ensuring that the data being monitored is always relevant to the practice’s goals and priorities.Proactive Care
BI tools like Power BI make it easier to adopt a proactive approach to care. For example, practices can set up alerts for high-risk patients or flag patients due for annual reviews. This ensures that practices can intervene early to prevent more serious health issues from arising.
Conclusion
In an age where data is increasingly at the heart of healthcare, the ability to harness and analyse information effectively is crucial for general practice. Power BI provides a powerful, easy-to-use tool that can help practice managers and clinicians unlock the potential of their data, ultimately leading to better patient care, improved operational efficiency, and stronger financial management.
As more practices adopt BI tools, we are likely to see a shift in how healthcare is managed, with data-driven decisions becoming the norm and leading to a more personalised, efficient, and proactive approach to patient care. For practices looking to stay ahead of the curve, investing in tools like Power BI is not just an option, but a necessity.
Power BI offers general practices an unprecedented level of insight into their data. By tracking a wide range of clinical, operational, and financial indicators, practices can transform how they deliver care, ensuring that decisions are data-driven and patient-centered. Whether it’s optimising appointment utilisation or improving chronic disease management, the potential of business intelligence tools like Power BI is vast, helping practices stay efficient, compliant, and focused on delivering better patient outcomes.
By integrating Power BI into daily operations, practices can transform how they monitor and improve performance, ensuring they deliver the highest standards of care while also optimising their resources. The future of healthcare is data-driven, and BI tools like Power BI are leading the way.
Please share this article if you like it!
I’m a fitness enthusiast and Peloton addict who loves challenging limits through races, paddleboarding, and life’s adventures. Here, I share milestones, reflections on Acoustic Neuroma, and stories of resilience and growth.




No Comment! Be the first one.